Wondering if you need a biopsy to diagnose Celiac Disease? Dr. Stephan Wangen has the answer, plus details you need to know.
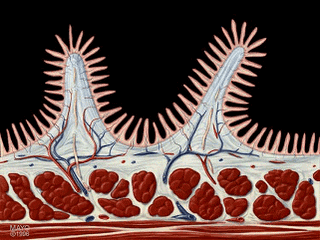
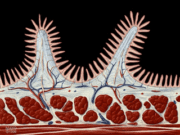
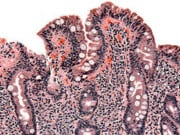
Celiac disease is traditionally diagnosed with a positive biopsy of the small intestine. The biopsy will demonstrate damage to the intestine known as villous atrophy. Villi are small finger-like extensions of the lining of the intestine that are visible only under the microscope.
People with celiac disease and other conditions will show a marked reduction in their villi, almost as if the villi have been worn off. Damage to the villi causes a dramatic reduction in the surface area of the small intestine, resulting in both the poor digestion and absorption of many nutrients.
Biopsies are done in a hospital on an outpatient basis, but require strong medication due to the invasiveness of the procedure. An endoscopy is performed, which involves a tube being placed into the mouth, down the esophagus, and past the stomach. A tissue sample can then be taken from the small intestine.
Although the small intestine is extremely important to our health, in most cases the value of the biopsy in diagnosing celiac disease is highly questionable. About 98% of people with a gluten allergy or celiac disease can be diagnosed as being allergic to gluten with blood tests alone.
There is no added benefit from performing the biopsy. The results of the biopsy do not change the form of treatment nor the outcome for the patient. Only if the blood tests are negative can a biopsy potentially provide useful additional information.
Article Courtesy: Dr. Stephen Wangen




Let Us Know What You Think